Anderson [1] describes a succinct history of pharmacy, charting it from early periods to the present day. He describes how the Sumerians in 2000 BC were using plant drugs and during the reign of King Hammurabi (1795�1750 BC), a system of laws, known as Hammurabi�s Code, was established. Medical and surgical practices were regulated, and diagnosis and treatment were separated from the preparation of medicine, which were carried out by assistants or apothecaries. A primitive understanding of drugs enabled formulations of draughts, mixtures, infusions decoctions, medicinal wines, ointments and poultices. Some are still in use today (myrrh, poppy, thyme, liquorice, peppermint, cannabis etc.). Around 1500 BC, the Egyptians had advanced practice beyond the Assyrians. In Egyptian society, diagnosing and treatment of illness was separated from making medicines, though pharmacy was regarded as a special branch of medicine. In Egyptian mythology, Thoth, the scribe of the gods, was known as ph-ar-imki (translated as �warrant of security�). This represents the origin of the word pharmacy.In ancient Greece, the word �pharmakon� was used for a process of cleansing or removing bad luck or circumstances. The pharmakon was often the person who was blamed for the ill luck and either cast out from the city or worse. However, the word was used in the context of people being made to feel better by a pharmakon. The key point is that for the last 4000 years across many cultures, while techniques and medicines have progressed, the considerations of professionalism, patient safety and use of latest developments are as relevant today as they have ever been.
�Electronic prescribing and robotic dispensing
In 2005, the UK Department of Health issued a report authored by the Chief Pharmacist �Building a safer NHS for patients: improving medication safety� [2]. This was a detailed paper on medication errors, the causes and potential remedies, and represented a development by the Department of Health from the paper �An organisation with a memory� [3]. The paper �Building a safer NHS for patients� made many suggestions on how errors could be minimised by designing them out through the use of a system�s approach to medication systems. In the paper, the use of electronic prescribing (EP) and robotic dispensing (RD) was put forward as potential tools to help reduce dispensing errors. The problem is that the use of electronic prescribing and robots is not systematically documented in the literature as to what features provide the greatest safety. There is a variety of design in EP and robotic dispensing systems, and it is important when surveying the literature to consider the context of the medication system in a hospital. For example, literature from the USA has a different pharmacy model in contrast to the UK, [4] where payment for services is through insurance and not state funded.
This means in the USA, tracking cost for re-charge to insurance companies is an important component of activity, and unit dose dispensing is much more of a feature of US hospital pharmacies. This is not the case in the UK, which needs to be remembered when looking at published literature.Karsh [5] commented that generally, health care was poor at implementing new technology to patient benefit. In the UK, over 400 (2010) dispensing robots have been installed (source ARX Ltd.), but the literature does not identify all the potential benefits the robots may give. The installation of so many machines in hospitals implies that buyers not only envisage benefits but also efficiencies in the dispensing process, since there is also potential benefit with regards to skill mix adjustment in the dispensary.Electronic prescribing (EP) is a subject that has produced many papers in the literature, but many of the studies originate in the USA and reflect to some extent the American hospital pharmacy model. Medication errors are a primary focus of reports in the literature with little focus on other aspects and benefits of EP. There are fewer publications on robotic dispensing, and a paucity of information on combining both EP and robotic dispensing, which would be of a wider interest to pharmacists generally.
Benefits of electronic prescribing (EP) and robotic dispensing (RD)
When considering the possible benefits of combining an EP system and robotic dispensing together, certain criteria need to be satisfied to yield the maximum benefits to the pharmacy, patients, to hospital organisations and indirectly to the value of the profession. These are as follows:
� An integrated EP system throughout the hospital to allow flexibility of working points and minimising re-keying of data and making relevant patient data available anywhere in the hospital. In this context, integration means the EP system links to other modules of the hospital systems, such as the patient administration system, the pharmacy system, pathology system, nurse administration system, chemotherapy medication system and so on.
� If a robot is used in the pharmacy, it is better that it is directly linked to the EP system to increase efficiency (avoidance of re-keying). Hospital pharmacies will generate hundreds of thousands, if not a million-plus, of labels a year, and re-keying data (to produce labels) can add up to a significant amount of time. The system also requires automatic labelling to maximise the benefits. Integration across hospital departmental systems also potentially permits use of pathology results to link to drug selection and prescribing. For example, a low white blood cell count may be a useful screen prompt when prescribing methotrexate. However, there needs to be care when considering such types of screen prompts, as information overload to the prescriber will have a tendency to render key messages likely to be unheeded.
� As the above criteria are met, resources will be released internally in the pharmacy to allow working processes to be re-modelled to perhaps focus to a greater degree on ward-based activity.
� The use of EP to do the �policeman� functions of formulary management means there are opportunities for enhanced professional relationships with nursing and medical staff, where pharmacists can fully utilise their clinical skills. This happens because EP can be operated restrictively, and this can be used to prevent doctors prescribing �off formulary�. The un-rewarding (and potentially challenging) task of changing what doctors want to prescribe is removed. The pharmacist is no longer a formulary policeman but the professional who helps prescribers navigate the EP system. This positive element to the work helps in ward relations and helps embed pharmacists in ward processes.
Benefits will be harder to realise at the ward level unless the pharmacy department has enough pharmacists with the clinical skills to deliver an enhanced professional role. Well-trained pharmacists are crucial to the whole process, and unless pharmacists are capable of delivering the service medical and nursing colleagues expect, technology implementations will under-deliver on wider benefits.
� Using automation technology does not denigrate the role of more mundane medicine distribution and procurement. If anything, it enhances it if wisely implemented, and skilful use of technology can reduce the number of staff needed to be involved in this activity (within the confines of the pharmacy walls at least).
� By doing more �higher� professional activities and less mundane work, the level of patient centred expertise of pharmacists and technicians is expanded and enhanced.
� Enhancing the clinical service into the broader aspects of hospital speciality activities increases potential pharmacy identities and potentially adds to the survivability of the pharmacy service. The impact is necessarily not only on pharmacists but also on other pharmacy staff. The potential for a wide range of electronic systems (EP, RD, �smart� �drug cupboards�, etc.) in the pharmacy means technical and other supporting staff is presented with new opportunities too. The developments in technology allow new roles for these staff in supporting these systems and developing expertise to maintain them. As such, these developments (along with ward-based activities) replace more traditional medicine preparation skills.
It is not an inevitable consequence of automation and deploying technology that an enhanced service will follow. Planning is required to make this happen. Some hospitals could choose to use the efficiency created to reduce the number of pharmacy staff employed. If this was the corporate decision, there would be no enhanced clinical service but that would be the organisation�s choice. The technology creates the efficiency, what happens after that depends on competing priorities at a corporate level.
However, should a pharmacy department look to implement EP-RD systems, the type of robot chosen may limit efficiencies, and the integration levels of the EP may also put constraints on efficiencies. The pharmacy management team must also think of the end game of any implementation programme. They must have a vision of what they want once the systems have been built. The pharmacy team needs to have a clear strategy of what the EP-RD system would be used to support and further develop the clinical service, which means that there has to be pharmacists suitably trained to be able to move into roles that the freed time allows.The �Building a safer NHS� paper [2] quoted a study from the dispensing error analysis scheme (DEAS) published by Cardiff and Vale NHS Trust [6] and analysed errors from 66 contributing hospitals from 1991 to 2001 and which included 7000 errors. As such, it represents one of the biggest surveys of its kind in the UK. The following categories of errors were recorded by frequency in Table 1.
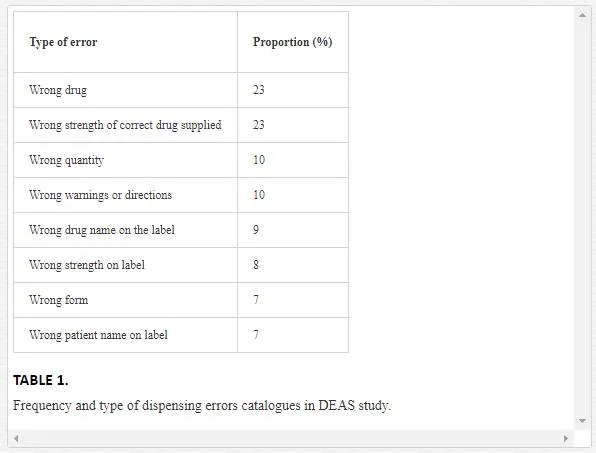
This profile of errors provides a plan with which technology can be adapted to remedy the potential dispensing errors. With regards to the UK, several authors have commented on robots in the UK pharmacies. In 2004, Swanson [7] described all the various types of dispensing machines from the chaotic storage type of ARX machines to the channel fillers produced by such companies as Baxter. Whittlesea and Phillips [8] described the efficiencies expected and the fall in error rates associated with robotic dispensers. No figures for errors were quoted, and the non-robotic dispensing rate (i.e. using staff) was quoted at 10 items per person per hours. James [9] looked at workload in non-robotic and robotic environments. She quoted a non-robotic dispensing rate of 7.25 items per hour and a robotic dispensing rate of 12 items per hour. She also quoted a dispensing error rate of 637 items per 100,000 for the manual system and 338 per 100,000 for the robotic system. The data did not specify if this only referred to items moved into the robot. Goundrey-Smith [10, 11] quoted a 50% error rate reduction at Wirral Hospital on installing a chaotic storage robot and a 16% error rate reduction with a channel-filler robot at Wolverhampton post installation. However, sometimes in papers, key features of the technology are not described, so it becomes difficult to assess what features are the most important in achieving tangible benefits. Cantrill et al. [12] looked at three types of EP systems in North West England. They surveyed medical and pharmacy staff and concluded on the basis of the surveys that the benefits of EP were difficult to quantify.
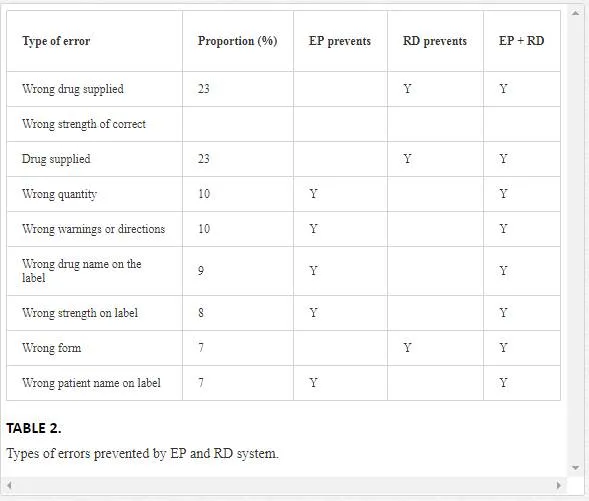
Reference to the appendix in the paper [12] outlines the functionality of the systems being used in the surveys. It becomes clear that the systems used were not integrated as described in this text and therefore not surprising that enthusiasm for EP across organisations was variable. The paper is a good illustration of understanding how the levels of functionality can affect benefits and perception of benefits. In some cases, some doctors were using dual systems (i.e. a �Kardex� and also an EP system), so it is not surprising where they are required to do more work, they become less positive about the technology. However, when looking at the potential for technology to assist in reducing dispensing errors, we can consider the DEAS error profile, and see how technology can have an impact on reducing dispensing errors.The following table identifies the potential error rate reduction potential of integrating an EP and RD system together.It follows from the analysis of Table 2 that provided the EP and robotic dispensing are integrated in a specific way, many dispensing errors can be �designed out� by skilful application of technology.
The key points to remember are as follows:
� Because EP system is integrated, when the doctor prescribes the medicine on the computer, he is also in fact writing the label to attach to the medicine. This means the label is always what the doctor requested.
� Because the label is always accurate to the prescription so there is no labelling error.
� If the RD system is used to store medicines by bar code, then drugs can only be supplied by the robot by bar code identification. There is then a direct electronic link between the medicine, bar code and item selected on the electronic prescription and the label that is printed. This is the most crucial step in deriving safety benefits from the technology. It is achieving this direct link through integration of the technology that delivers safety benefits. To design in these links is to design out potential errors.
� Once so designed, the system works from anywhere in the hospital. This allows significant amounts of dispensing activities to be triggered outside the pharmacy, but only works if there is a direct link between prescription, label and robot.
� Automatic labelling is a critical component of this system.
� Once medication has been checked by a pharmacist in the EP system, it is possible to make the dispensing nearly instantaneous. The remaining bit of the process is to get the medication from pharmacy to the ward promptly.
� In achieving �instantaneous dispensing�, the role of the pharmacist potentially changes. No longer are pharmacists directly in control over the whole dispensing process. It is akin to craftsmen producing goods being replaced by production lines where quality control is through process control, and each individual is responsible for a part of the overall process, not all of it. This has some significant implications for the way the pharmacy is subsequently managed and run.
A skilfully designed system should produce zero errors for the robot plus EP system combined, potentially a huge benefit in safety. This is far better than quoted in the literature for robotic dispensing [8�10] and should be regarded as significant. The system design prevents errors. A key feature of this is an automatic labeller, which means there is no point in the dispensing process for human intervention, and crucially, potential human error. Because of the EP system, no re-keying of data is required, so the process becomes more efficient.Dispensing rates can be significantly faster than quoted in the literature. However, dispensing in the pharmacy is not entirely risk-free, since not all items are supplied and labelled from the robot (for example, oral chemotherapy). Clearly though, the opportunity for errors is significantly reduced.
When compared to the system outlined by Reifsteck et al. [13] and Gonidec et al. [14], the comparisons start to encounter the contextual difficulties of understanding the medication systems in other countries (in these cases, USA and France). Reifsteck describes his hospital as having 900 beds and says his hospital in Albuquerque consistently ranks among the top ten integrated delivery networks in the USA. They use computerised practitioner order entry (called EP in the UK) and integration with a unit dose pharmacy robot. The hospital in the USA also has a closed loop patient administration system. Gonidec et al. [14] describe the use of a robot combinded with electronic prescribing in a French prison (for 700 prisoners). They used a unit dose system similar to quoted by Riefsteck [13]. Gonidec quotes an error rate of 0.5% post implementation, but these are quoted as mainly wrong location delivery of orders triggered by the EP system. Gonidec also quotes a production rate of 377 doses per hour and the types of error and the number of times they occurred in the 3-month study, but they bear no resemblance to the DEAS study and relate to operational problems within the unit dose system.
Reifsteck et al. [13] quote a drop in error rate from 23.5% pre-automation to 9.9% post automation. Their figures include wrong time administration errors (defined as being plus or minus 1 hour of specified time). When administration errors are not included, the rate falls to 1.9%. Nowhere in the document are dispensing errors mentioned. Without wrong-time administration errors, there were 10 errors logged, 7 being wrong administration techniques.
Potential methods of evaluating EP-RD
TURN AROUND TIME FOR PRESCRIPTIONS
There is potential within an EP-RD system to increase the speed of turnaround time from the point of the clinical check of the prescription to nearly instantaneous, which is not a common feature within substantial numbers of UK hospitals at present. However, at very busy periods, the dispensing times can potentially rise, depending on the capacity of the RD system chosen. In traditional �Kardex� hospital systems, dispensing times can often be up to 4 hours for non-urgent dispensing [15]. Beard (no relation to this author) and Wood quote how, by using �Lean� processes, they reduced the dispensing time of the prescription from 4 h to around 1 h in a pharmacy which had robotic dispensing (these times include the time it takes a signed prescription to get from ward to pharmacy).
DISPENSING RATE
Whittlesea and Phillips [8] and James [9] quote benchmarks of around 10 items per person per hour. The linking of EP and the robot means there is an efficiency increase, simply because of avoiding re-keying in data. Dispensing times can have a potentially significant fall. This efficiency does not compromise on safety. The EP component of the system gives in effect a huge digital capacity compared to a traditional Kardex-based system. The robotic component adds significant picking and mechanical capacity and is limited only by the limits of what can be configured in a particular dispensary. The potential dispensing rate is then only limited by the number of picking heads that are deployed.
OUT OF HOURS SUPPLY
The automation of supply of products means that anything that is in a robot could be supplied remotely. This feature is used in many hospitals in the UK. A night safe can be built into the pharmacy to allow nursing staff to collect items sent to the night safe chute. The on-call pharmacists could have remote access to the software via a hospital laptop and also have access to the patient�s prescription and other relevant data (e.g. pathology) via EP. Supplies, if appropriate, can be made out of hours without the pharmacist attending. While this is an attractive feature, there is a potential downside in that the convenience of such systems creates the potential for work �drift� from wards from normal dispensing times into times that are intended for emergency or urgent needs only.
Ï¿½RETURNED STOCK
There is a benefit opportunity from robot installation to make it easier to manage stock returned which could be re-issued if an automatic loading hopper is a part of the RD system. The effect is more a staff behavioural one rather than direct effect, but if ward�s stock is returned, prior to robot installation, there is work required by the store or dispensary staff to put the items back on the shelf. Even if it is just a few packets of different items, it can require a relatively large amount of work to put these items back on the appropriate shelf. With the robot hopper, it is relatively easier and less time consuming for staff to put these returns on the loading hopper and re-using the products is made easier. All store or dispensary staff have to do is put returned stock on the conveyor, and the robot does the rest. Because it is easy to re-cycle stock, stock is re-cycled and wastage potentially falls. However, the benefits of this aspect depends on where a hospital pharmacy already is with regard to its current stock re-use, but an automated loading hopper should either permit greater increase use of returned stock or allow less staff to be used in this process.
Ï¿½EXTENDED HOURS OF SERVICE
As the EP-RD system increases efficiency, it should facilitate the manning of addition hours easier, as less staff should be needed in the dispensary than would be required in there were no such system. As such, the EP-RD system would reduce the cost of providing an extended hour�s service by reducing the manpower needs (in the dispensary at least). Outside normal working hours, staff (covering late nights and weekend shift workers) may not be as familiar with stock control methods and be tempted to take supplies from shelves without recording them. Each individual may think it is only one omission, but the compounded effects over time can thwart the re-ordering algorithms, leading to a tendency to overstock �just in case�. By installing a robot, it potentially denies access to the robot shelves, and forces staff to follow standard procedures, making the stock recorded on the computers more accurate.
All of the above identified benefits have a significant impact on the efficiency of the pharmacy. The cumulative effect is to make the dispensary processes more efficient. This frees resources for other work and can create a means for significant departmental developments. These are summarised in Table 3.

Implications of EP-RD on the professional model
As a result of implementing combined integrated EP and RD systems in the pharmacy, it becomes apparent there are further implications for pharmacy beyond operational efficiencies. The professional model potentially can be changed or developed further, and professional identities for all pharmacy staff can be modified.One implication of the EP-RD model is the dispensary pharmacist �oversees� the supply of dispensed medicines leaving the pharmacy, but he may not have seen many of the prescriptions and has not had any sight of the dispensing process. This can be because his pharmacy colleagues are doing the dispensing process controlled from ward level though the EP-RD system. He is faced with a series of labelled packets for patient X and trusting that his colleagues have all done their part at ward level, permits the dispensed medicines to be dispatched to the ward.
Ï¿½IMPACT ON LOCUMS
One consequence of changing the operational model is the training time required to get new members of staff competent to work with EP-RD systems. Some sites report it takes around 3 months for new staff to gain enough knowledge to be confident of using an integrated EP-RD system at a competent level. This has implications for ensuring proper induction of staff when starting, requiring staff available to manage the training process. It also has a potential negative effect, which means that the short-term locum cover is not really possible. Locum pharmacists are very much part of the pharmacy profession, providing cover when the regular pharmacist(s) are not there. In the traditional model, because their expertise is focused on the paper prescription, whichever pharmacy they are in, they can clinically check the prescription and check for accuracy. In the EP-RD model, they have to be trained in the systems to find the electronic prescription and know what functions to use to provide the clinical check. Because the electronic system is highly integrated, all the information a pharmacist needs is available within the computer (pathology tests, nursing notes, radiology reports, clinic bookings, previous admissions, etc.), but the pharmacist needs to know where to find all of this information. The consequence of not being able to use locums means that as a department, the hospital pharmacy has to have a process for replacing staff that leave with a system of timely succession planning.
SKILL MIX
The installation of an EP-RD system could trigger efficiencies with regard to skill mix in the dispensary. This is because in an EP-RD system, there is no need for interpretation of the doctors� handwriting (since prescriptions are electronically written); it is possible to de-skill the activity of dispensing and checking, since the professional check now becomes mainly a process check.
OTHER PARAMETERS
As mentioned above, other parameters of efficiency may become possible such as stock holding, stock turn, dispensing error reduction, speed of dispensing and stock re-cycling. The impact of EP-RD should show improvement. This frees pharmacy staff, both pharmacists and technicians, to be potentially deployed in ward areas and other clinical settings.
�Taxonomies in other disciples; mapping a taxonomy for hospital pharmacy
It may be worth considering if the EP-RD model changes the professional model of pharmacy? If so, what are the implications for the future? Is it likely to have a positive or negative impact on the profession? Will it increase professionalism, reduce it or be neutral?
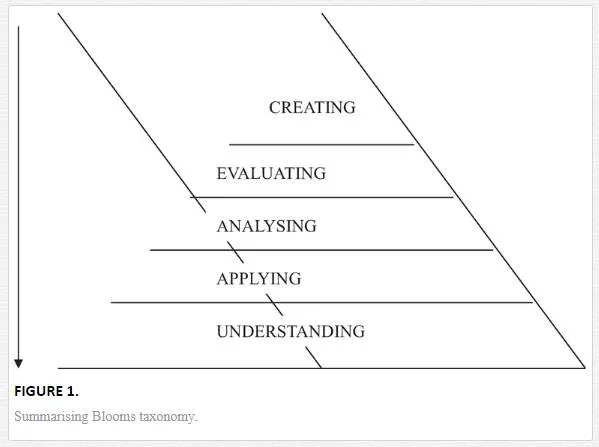
Looking at other taxonomical models may give some predictive insights. Bloom [16] laid down his taxonomy of learning. It is described in a hierarchy. Its aim is to summarise different thought processes to create continual sustained learning. This is summarised in Figure 1.
Similarly, this hierarchy model has been applied to informatics by Ackoff in the 1980s, when looking at methods to describe the relative value of information [17], as in Figure 2.

In Ackoff�s model, he carefully defines the words as:
� Data = symbols
� Information = processed data
� Knowledge = applying data and information (how questions)
� Understanding = Appreciation of �why�
� Wisdom = evaluated understanding
The significance of the top level is that it represents a better capacity to manage an environment. As Ackoff pointed out, organisations ought to become �wise� because it confers potential sustainability of the organisation. It permits the better survival of the organisation. Goundrey-Smith in his text [10] describes a similar �Bloom� style of hierarchy for electronic prescribing systems and is summarised in Figure 3.
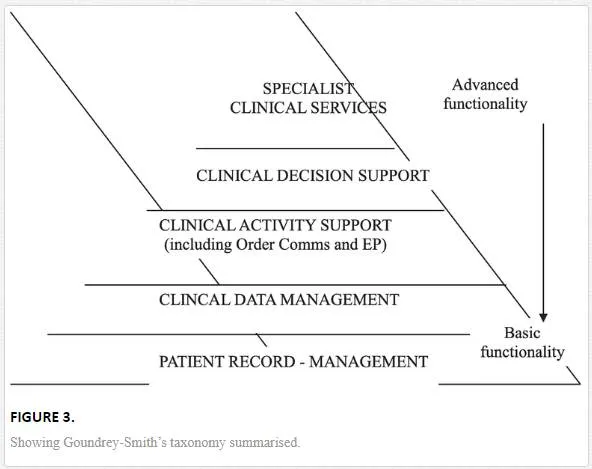
The hierarchy Goundrey-Smith describes for electronic prescribing has similarities to Ackoff�s model. The assessment for technology and its impact on professionalism could be mapped against pharmacy activities, to provide more details of practical use. If we look at hospital pharmacy activities, we could list them as: Procurement, distribution, dispensing, ward stock supply, out-patient services aseptic manufacturing, non-sterile manufacturing, medicine information, audit, clinical services, running clinics, clinical trials activities, research work, R&D work, management functions, weekend services, on-call services, attendance to interdisciplinary meetings, finance work, reporting to within organisation, staff induction, staff training, record keeping and controlled drugs management. These are described in Table 4.
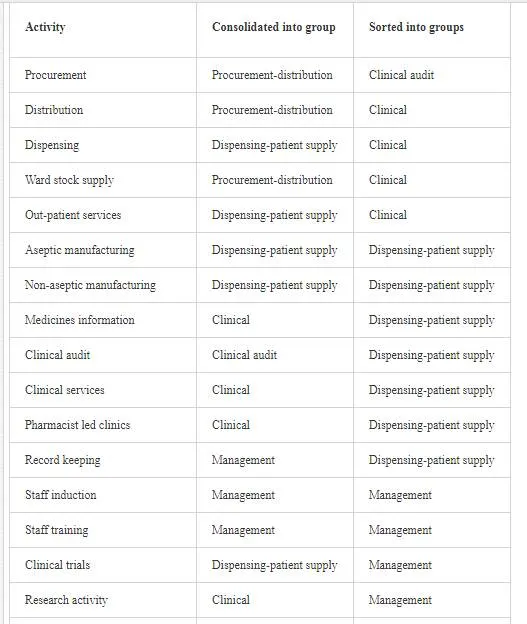

Most hospitals in the UK will undertake all of these activities to a greater or lesser degree, and the relevant proportions will depend on local circumstances range of specialist services, number of beds in acute hospital etc. The proportion of time relative to their activities by staff might provide a useful indicator. The hierarchy is based on the skill levels of NHS Pharmacy staff routinely undertaking these functions, and this could be reflected in the pay band, which is heavily weighted to qualifications.
1. Specialist clinical service
2. Clinical service
3. Management
4. Dispensing-patient supply
5. Procurement-distribution
Do these functions exhibit any similarities to Ackoff�s or Bloom�s model? The taxonomies are summarised in Table 5.

Superficially, there seems to be similarities with Bloom�s than Ackoff�s model. However, the real insight comes when the normal amount of time spent on these activities is considered, which can be used as a comparison tool. This starts to lay the basis of assessing the level of �higher� professional activity.
This method of assessment might be useful for comparing different hospital pharmacies, but the real value of it is in telling an individual pharmacy manager where they might be in terms of how much �higher� professional activity is going on within a department and what impact implementing technology might have on higher professional functions. Why is this important? Because some surveys indicate that pharmacists feel empowered and have better ward relationship within an EP-RD model. It allows them to �cover more ground� and enhances professional relationships. Using EP and robotic dispensing potentially reduces the level of dispensing done by pharmacists and therefore moves more towards the apex of the professional pyramid. It does this by reducing the amount of time spent by pharmacy staff on moving medicines about the hospital, thereby releasing staff for other higher skilled work.
These are all strong benefits, both to the pharmacy and patient care and therefore to the organisation. Using the descriptors of the higher elements of Ackoff and Bloom, technology enhances the �wisdom� and �creating� levels, increasing the value the pharmacy adds to the organisation. It is in the process of adding extra value to the work done within the pharmacy within resources that makes the service more valuable to the organisation.
The literature raises a further issue. Nation et al. [18] make the point that in the literature there are no common terms used for describing medication errors, and that this makes comparisons in the literature difficult. Goundrey-Smith [10] notes the differences in terminology of EP in the UK and �computerised physician order entry� (CPOE) in the USA. He points out that the terms are often used synonymously, but that CPOE is a broader term which includes EP, but encompasses transmission of other clinical order types, such as pathology tests or radiology tests. Across Europe, there is a standard that looks at EP in health informatics (European Committee for Standardisation, European pre-standard (ENV Health informatics); messages for the exchange of information on medicine prescriptions). However, these standards are more to do with message design. There still remains the problem of describing levels of technological functionality across publications. Taxonomies are a means to clarify things or concepts and have an underlying principle for the classification. Castillo et al. [19] did an extensive literature search to look at factors that made physicians use an electronic health record. They identified from their literature search six factors: user attitude towards electronic systems, workflow impact, inter-operability, technical support, communication amongst user groups and expert support. These were defined as the critical adoption factors. However, 55 of the 70 papers reviewed were from the USA, putting a contextual bias to the conclusions. Some UK experiences do not reflect the Castillo et al. [19] view with regards to their six main factors; nor should it. Bell et al. [20] identified 9 EP capabilities. Again, it is a USA-based paper and reflects their context. They proposed five activities in the prescribing pathway that needs to be included in a system. These are as follows:
� prescribe
� transmit
� dispense
� administer
� monitor
From this, they proposed that an out-patient EP system should have the following capabilities: patient selection, diagnosis selection, medication regime selection, safety alerts, formulary alerts, computer assisted dose calculations, transmission to pharmacy (pharmacies) administration and monitoring.
When assessing the literature, there is a problem with regards to evaluating reports of electronic prescribing and dispensing robots. The study by Cantrill et al. [12] looked at EP in three different hospitals in the North-West and assessed the doctors� and pharmacists� views of the benefits of EP. The surveyed hospitals had three different systems. Functionality in the systems was described, apart from the listing in the appendices, but no comments were made regarding the impact of the EP functionality on the results. In reading papers on EP and RD generally, some implicit knowledge of the subject is required because of the lack of common terms for his subject matter. A reader of the Cantrill et al. [12] study unfamiliar with the subject might be misled to regard there being little benefit in developing EP systems in hospitals because it does not consider the impact of different levels of functionality that framed the feedback from pharmacists and doctors.
Another consideration is that as pharmacists become more ward based, they potentially loose dispensary skills. Within EP-RD systems, it is more practical to have staff trained to manage and maintain these systems, but they are not necessarily pharmacists. Technicians can be managing these technical activities. Technicians were taught traditional dispensing skills, but these skills are used much less nowadays. However, as pharmacists move out to the wards, dispensary management, robot management, procurement, IV fluid management and EP dictionary maintenance can be technician led activities. Technology adoption not only increases the potential for increased pharmacist professionalisation but also pharmacy technicians. Technology potentially expands roles (altered boundaries as Barrett et al. put it) [21] but in a positive way. The effect trickles down to non-technical staff. It is possible to create in the UK NHS staff grade structures a clear qualification-based access scheme to allow band 2 staff (unqualified) to become qualified to become band 3 (dispensers), thence to band 4 (basic technician), to band 5 (medicines management technician) and thence to supervisor roles (band 6). This system can be used in part as succession planning to fill vacancies as they arise. It is also cost effective, as replacing a band 5 staff member may only cost after staff have shuffled up a grade a band 2 replacement, as far as the staff budget is concerned. This is a useful rationale when negotiating vacancy replacement with higher hospital management.
The introduction of technology into (health care) professional settings needs to be taken seriously, especially from the perceptions of those who interact with technology as it has the potential to regulate, mediate, govern and represent health care professionals, altering both what they do and who they are. These alterations are neither unidirectional nor deterministic. Health technology opens up a field of multiple possibilities for both re-professionalisation and de-professionalisation. De-professionalisation (e.g. as mentioned above, de-skilling the dispensing process) is conditioned upon four main IT enabled possibilities. First, through automation, technology alters the nature of professional work by shifting its temporal, spatial and manual aspects. Technology through electronic connection has the potential to expand professional boundaries to other occupational groups working at ward level. Pharmacy is no longer just a building on the hospital site that stores medicines, but a comprehensive service every bit as visible as nursing or medical care. Technology enables re-professionalisation in three ways as follows:
� Through automation it undertakes mundane tasks and gives health care professionals the opportunity to undertake more challenging mental and clinical activities in their everyday work.
� By digitalising, transferring and translating information, it expands pharmacists� jurisdictions (through the creation of new or the reshuffling of old responsibilities) and gives them the chance to exercise more discretion and professional judgement.
� Finally, through electronic connection and identification, technology expands professional boundaries by allowing professionals to become a more integrated part of the ward teams.
While there is some agreement about what constitutes professional behaviour, there are no published concepts of what is the professional model in pharmacy or what constitutes a �higher� professional model. In Canada, Motulsky et al. [22, 23] looked at the impact of technology on professionalisation of community pharmacy and concluded that the adoption of technology increased professionalisation. They defined increased professionalisation as pharmacy practice centred on clinical activities within pharmacy services. The literature abounds with papers written on EP and also on robotic dispensing, but there are few instances where the impact of both together is described. The study by Reifsteck et al. [13] in the USA is a notable exception. There are fewer papers exploring the impact of technology on professionalism within pharmacy. There is also some confusion in the literature regarding what constitutes electronic prescribing, which distorts benefit analysis. This identifies an emerging need for a common language to describe the technology to be able to better compare studies in the literature, akin to Nation et al. [18] call for a common language in medication errors.
Much debate has taken place over what constitutes a profession, a professional, and the concept of professionalism [24�32]). Sociological theorists in the 1960s and 1970s challenged occupations with professional status and the monopoly they hold over society [33, 34]. Denzin and Mettlin in 1968 accused pharmacy of being an incomplete profession based on criteria established by the Trait theory. However, the approach of the sociological theorists could itself be challenged, as the law is quite specific what constitutes a profession: a profession has a registering body, has a code of practice and enforcement arm of the registering body. Breaking the codes of practice can result in being removed from the professional list and unable to practice. This pragmatic assessment seems to have been overlooked by the sociological theorists. However, Pharmacy was labelled (dubiously??) as a quasi profession, in as much it had some but not all characteristics of a profession [27].Technology opens up a number of, often contradictory, possibilities for shaping pharmacy professionalism but does not determine it. Professionalism (and hence professional satisfaction) is conditioned upon the way in which professionals will exercise their power. The consequences technology imposes on professionals has important implications for how pharmacists use (or not), adapt and adopt technology and points towards an exploratory perspective that looks into how and in what ways technology may shape health care professionals in the future. This has always been a historical tradition, as Anderson�s history of pharmacy points out [1].
It becomes apparent that there are implications regarding using the technology and the possible impact on professionalism. The historical summary taken from Anderson�s �History of Pharmacy� frames aspects of professionalism noting that since from 2000 BC, Pharmacy has always been separate from Medicine and is recorded as such. The American Board of Internal Medicine �Project Professionalism� [35] document and also a similar UK document published in England in 2004 by Rosen and Dewar [36] were both designed to address the teaching of professionalism to undergraduates, against a background that public confidence in the profession needs to be maintained. Similarly for pharmacy, the American Association of Colleges of Pharmacy Council produced a document in 2000 [37] to ensure pharmacy students were taught professionalism in schools of pharmacy, and in the UK, Schafheutle, Hassell Ashcroft et al. produced a similar document in 2010 [38]. These papers were responding to a perceived need, but the earlier publications of these papers in the USA suggest the health care systems in which they operate triggered the need earlier. This might in part be linked to a health care system not free at the point of delivery, but insurance driven, and the need to demonstrate the professions was using expert skill for patient benefit and not exploiting a monopoly situation for their own rewards.
The problem for Pharmacy is that EP and RD developments happen outside the Universities where undergraduates learn their skills, and the opportunities technology creates provides a wide range of opportunities for the profession to develop. The potential to significant increase the efficiency of the dispensing process provides a springboard for increased ward activity. The use of EP to �police the formulary� removes a small conflict task done by pharmacists, permitting a more positive working relationship with other ward professionals. The potential for reducing the cost of extending the working week in terms of staff numbers also increases availability of pharmacy staff and creates further roles and professional identities for staff. Future digital developments create potentially new professional identities and further develop professional boundaries. The development of an EP-RD system is not only an end in itself, it is potentially a gateway into a more comprehensive and diverse future for all pharmacy staff.


